Thanksgiving Harm-Reduction Steps for Those Who Will Travel or Gather Anyway
There is no way to eliminate risk, but anything one does to reduce it is better than nothing
Millions of Americans are traveling for Thanksgiving. In doing so, they’re increasing the chances of catching or spreading Covid-19—not just themselves but to others. A wedding reception in Maine ended up causing 177 cases and seven deaths—but none of the deaths were among people who attended the wedding, but rather, among their contacts.
It’s never too late to decide not to travel or choose not to meet with large groups of people not in one’s household during the holidays. There is excellent news regarding vaccines and therapeutics, and we may be very close to turning the corner on this pandemic. One can always have Thanksgiving in spring and be grateful for having survived a pandemic! As I recently wrote in The Atlantic, it’s time to hunker down!
The good news—we are so close to the beginning of the end of this pandemic—makes it especially important to try to safely get through this last terrible coronavirus surge.
I’d especially urge people to consider that hospitals are running out of not just space, but of qualified people. This report is a sobering read from a hospital that was otherwise very-well prepared. We can expand space within facilities and even set up field hospitals. But there is no way to mass manufacture doctors and nurses. With a nationwide surge underway, workers from one region cannot travel to bail out another, as they were able to in spring. Keeping infections down means that hospitals can do a better job taking care of the already overwhelming numbers of people who need care.
Nonetheless, the reality is that millions are traveling. Remember: one really cannot meet with other people at zero risk. But there are methods to reduce risk. And if we’re already taking risks, it’s better to reduce those risks as much as possible, rather than assuming that once we’re disregarding CDC advice, we may as well throw all caution to the wind. (It’s still better to take CDC’s advice!)
With that in mind, what are some precautions you can take if you do decide to travel or meet with people not ordinarily in your household? Or what can you tell people in your family or social networks who are doing so and you cannot persuade otherwise?
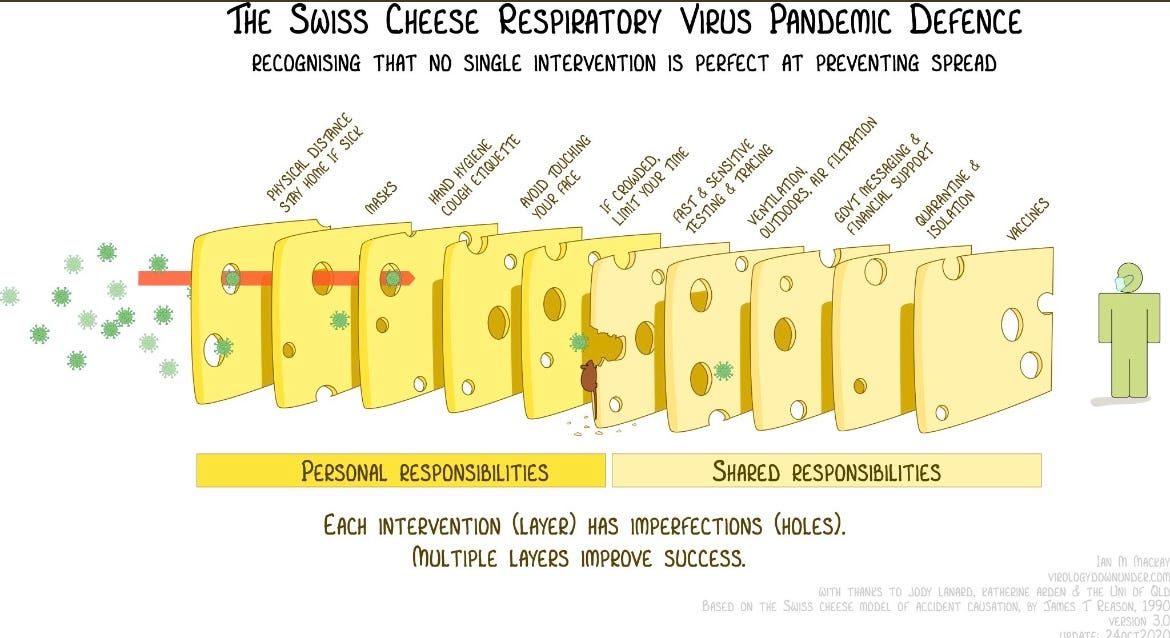
Remember that all mitigations layer and add up. I love virologist Ian Mackay’s conceptualization of the swiss cheese defense against the pandemic. The more layers, the better. Some layers are shared responsibilities, some are personal. The more we can all do, the better everyone—not just ourselves—will be protected.
A quarantine before any group interaction is the best preventive step, though of course it is too late to start one that’s long enough in time for Thanksgiving. If everyone in a given group was truly quarantined beforehand (two weeks is the standard period for a quarantine for Covid-19, but one week is better than none), the risk level is much lower for the meeting. Whenever you plan to meet others, quarantine beforehand is the single best risk reduction step you can take. While the longer the better, any amount of quarantine is better than none.
Also, keep in mind that if you travel via a method other than driving alone, you haven’t been properly quarantined. Still, even if you fly, take a train or bus, or drive while interacting with others along the route, you can reduce your risk. Any reduction in contacts with other people helps lower the odds of getting or spreading the virus. So if you are travelling, try to travel in a manner that limits contact with other people.
If you must travel in a manner that includes being around other people: consider wearing an N95 or KN95 mask whenever you’re around other people—you don’t need to purchase many. Indeed, you shouldn’t purchase many of these high-end masks, since healthcare workers still need them. But if you have such a mask, do wear it around other people, especially in places like crowded airport terminals, taxi rides or on planes. Don’t take it off if you don’t absolutely need to. It will make you safer from others, and them safer from you.
If you only have cloth masks, remember that their particular fit and layers matter.
Here’s some practical advice on how to make your mask fit better. Here’s good advice on how to wear a surgical mask better. Here’s guidance on how to best put on or take off an N95 mask. Here’s a tutorial on how to store an N95 or a KN95 in a tupperware container—just remember it should not be an airtight container. Punch some holes or buy those plastic containers with ventilation holes. (You can let the mask just sit there for a few days before wearing it again. Even if the mask was contaminated, the virus does not remain infective forever).
For cloth masks, consider these findings from a study just out from Virginia Tech prof Linsey Marr, and her team—she’s been consistently excellent, studying cloth masks as early as March. She’s among the top aerosol scientists in the world.
Combining the study’s findings with existing published literature on mask layering, Marr’s team came up with recommendations for fashioning a particularly effective homemade face covering: make it three layers, with a soft, flexible, tightly woven fabric layer up against the mouth; a layer made of material designed to filter particles, like a vacuum bag or MERV 14 filter; and finally, another soft and tightly woven outer layer of fabric. The face covering should fit snugly against the wearer’s face with no gaps that could affect its performance.
In addition, wash your hands often, or use hand-sanitizer. You may have heard that we do not have a lot of surface (fomite) transmission in the epidemiological record—but it doesn’t mean that surfaces pose zero risk. Hand-washing is a sensible precaution against many types of infections.
Once you have arrived at your destination, remember: ventilation and distance reduce the risk related to Covid-19. Even within a household, virus transmission is not inevitable. There are examples where people in the same household as a symptomatic person never get infected. Wear masks, especially indoors. Consider wearing them outdoors as well—especially if there is anyone high-risk in the group. Sit outside as much as possible. Hang out around a fire pit. Open windows as much as possible. Use a HEPA filter and run it at its highest setting. Continue to socially distance, especially indoors. Sanitize high-touch surfaces, especially if they are non-porous, like stainless steel fridge doors and door knobs.
There’s increasing evidence that humidity helps lower transmission. Keeping the house at 40-60% relative humidity is great, not just for this coronavirus but other viruses as well. Also, too much humidity can encourage mold growth.This virus may also survive better at high-humidity, as its reaction appears to be U-shaped. Purchase a humidity reader (available for less than $10) and keep the house at mid-range humidity levels.
Finally, give the best masks to high-risk people: the elderly, those with pre-existing conditions, and the immuno-compromised. Besides age, here’s a list of what’s considered highest risk for complications for Covid-19 :
Cancer
Chronic kidney disease
COPD (chronic obstructive pulmonary disease)
Heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies
Immunocompromised state (weakened immune system) from solid organ transplant
Obesity (body mass index [BMI] of 30 kg/m2 or higher but < 40 kg/m2)
Severe Obesity (BMI ≥ 40 kg/m2)
Pregnancy
Sickle cell disease
Smoking
Type 2 diabetes mellitus
Traditionally, communal eating is the center of Thanksgiving festivities. However, it is also one of the highest risk activities, as one cannot be masked while eating, and people tend to speak loudly around a table. Eating together doesn’t have to be the centerpiece of the day, though. It’s possible to eat separately and make the highlight of the day a different group activity. A gathering outside around a fire pit would be great, for example. It’s fun and, being outdoors, it’s safer, too. Playing a board game where people keep their masks on is another alternative. Keeping masks on is especially important for multi-generational gatherings, or for groups that include higher-risk people. The minimal set-up could be that the elderly could eat separately from the rest of the group. If they must join the dining table, they can do so while wearing the highest-grade mask they have. Risk reduction is important for everyone, but it’s most important for those at most risk. It’s much better to have a much more festive gathering in spring or summer, even if it makes this Thanksgiving a little more awkward.
Getting tested before or after a group meeting is tricky. On the one hand, of course testing is a good precaution to take, and a positive test result means you absolutely should isolate! However, one can test negative even while having Covid-19, because the disease hasn’t progressed enough—and then be infected and infectious just a day or two later. I wouldn’t consider a negative test a licence to do anything differently. In other words, even if you test negative, take all the precautions that you can: stay home and don’t travel for Thanksgiving, or, if you decide to do so, quarantine and take all the harm-reduction steps you can anyway.
The same precautions apply for the return trip: travel in the least risky way possible, keeping in mind that contact with other people poses the highest risks. When you return, quarantine. The gold-standard period for quarantine is two weeks, but don’t think in binary terms. Don’t think that if you can’t do two weeks, you may as well not quarantine. Two weeks is better than a week, a week is better than nothing. When you return, it’s best to act like you might be infected.
What if you get lucky by exposing yourself to a high-risk situation and emerging untouched by Covid-19? Don’t assume that your luck will hold for the Christmas season. Every encounter is an independent risk. There is no such thing as “a winning streak” with this disease. Getting lucky once is no guarantee of being lucky a second time.The changing winter conditions and the explosion in infections means that any meeting right now is much higher risk than before, when the weather was warmer and case numbers were lower. We now have three vaccine candidates with excellent results and vaccinations will start as early as December. We have effective therapeutics—they are in short supply but manufacturing is ramping up. We will have better weather once we get through this winter season. We are so close to the finish line. The more precautions we take, the better our chances.
(This email and web posting is open to the public, feel free to share if you think it may be helpful to anyone you know).


I had agreed to go to a small Thanksgiving gathering (there would have been 4 of us). We figured that with windows open, knowing we are all cautious about the risks of infection, it would be safe. Then I read your latest "hunker down" article :) I shared it with the hosts and they agreed it's just not a good idea to have an indoor dinner right now with different households. For context, we don't have cars so travel would be by subway and we live in apartments so we don't have backyards. If Friday is sunny, maybe we'll eat outdoors at a restaurant. BTW, nice touch that the url to the Atlantic article includes the phrase lock-yourself-down-now (!)
Thank you for this! I love the Swiss cheese model, but I have been pondering if there is a way to more effectively communicate a few important details related to COVID:
(1) There are three distinct "pathways" of exposure - aerosols, droplets, and fomites. Many of the risk reduction steps only address one or two of these pathways. So in essence you need to make sure you have some "slices" for each pathway. This is not well communicated by the "single pathway" model. For instance, the >6ft separation is only effective for droplets, not aerosols...
(2) I also think that along each pathway, there are three major categories -- source control (quarantine of exposed/infected individuals, etc.), environmental mitigation (cleaning surfaces, ventilation), and personal protection (masks). Moreover, some actions (do "double duty" -- e.g., masks are both source control and personal protection -- which makes them more effective!
(3) Finally, different actions have different effectiveness within their "cell" in this 3x3 matrix. For instance, temperature checks are intended for source control, but have low effectiveness due to asymptomatic transmission.
I've been struggling as to whether there is a way to effectively summarize and communicate this information in an infographic -- to encourage people to make sure they "cover all three pathways," to place their personal actions in context of community-level actions, and to understand the relative effectiveness of different actions.... or is it too late?